This is part of a blog series as we explore using Care Opinion in the last weeks and months of life, and in bereavement. It's co-authored by Jackie Le Fevre and Saskie Dorman.
You can read earlier blogs here.
Values inside stories
Individual stories shared by people through Care Opinion described some of the things that really matter at end of life and in bereavement. These powerful insights helped us to identify specific improvement opportunities, but we still wanted to explore further. Might there something about the way people tell their stories, that could connect us to what mattered at a deeper level; namely the level of their personal values?
We all have values and in general are unconscious of their presence. That said, we naturally notice both when values which are important to us are honoured, and also when they are not. This ‘noticing’ often takes the form of feelings.
For example, if someone notices “they answered the phone straight away and knew exactly how to find the answer to my query” and feels reassured by this it is possible that efficiency and knowledge are important to that person. “Nothing was too much trouble, the staff went above and beyond to make sure my wife felt well cared for” accompanied by a feeling of appreciation or gratitude - may point to generosity and care or nurture being priority values at this time.
What we did
To explore stories for values we first needed to choose a time period to analyse. We reviewed stories published on Care Opinion from September 2013 to end of August 2019.
August 2013 marked the publication of the independent review by Don Berwick: A promise to learn – a commitment to act: Improving the safety of patients in England. One of 10 recommendations was that:
“All organisations should seek out the patient and carer voice as an essential asset in monitoring the safety and quality of care.”
So our research started at a point in time when more attention within healthcare was being placed upon attending to patient and carer experiences.
Ending in August 2019 focussed our attention on experiences under ‘normal’ (not pandemic) conditions to create a baseline against which we could compare stories gathered during the lifetime of our project.
We used a specialist software, ValScanTM - built upon the Minessence Values framework - to map the values expressed in the stories and experiences people shared.
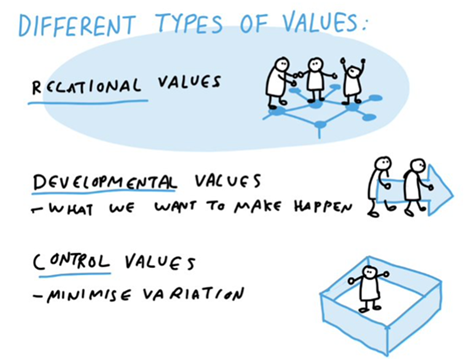
We focussed on three domains of stories; those related to end of life care, palliative care and palliative medicine. We combined the end of life and palliative care stories into a single data set and compared these to palliative medicine.
What we found
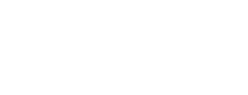
Here is a comparison of the most frequent high priority values contained within the stories in our study period. Relational values are shown in green; developmental values in blue; control values in orange.
End of life care / Palliative Care
Care/ Nurture
To be physically and emotionally supported by family and friends and to value doing the same for others.
Family/ Belonging
Having a place or sense of home. To be devoted to people you consider family and to experience belonging and acceptance.
Empathy
To deeply relate with others in such a way that they feel understood.
Generosity
To unconditionally share your resources, talents and skills as a way of serving others.
Interdependence
To value personal and inter-institutional co-operation above individual decision-making
Communication/ Information
The effective and efficient flow of ideas and factual information.
Community Support
To have, or to create, co-operative groups of peers with shared values that provide mutual support and enhancement of each other.
Education/ Knowledge
Engaging in ongoing learning to gain new facts, truths, principles and insights.
Health/ Well-being
To practise self-awareness and healthy living in order to have physical and emotional well-being.
Service/ Vocation
To use your unique gifts, skills and abilities to contribute to society through your career, profession or calling.
Palliative Medicine
Care/ Nurture
To be physically and emotionally supported by family and friends and to value doing the same for others.
Empathy
To deeply relate with others in such a way that they feel understood.
Family/ Belonging
Having a place or sense of home. To be devoted to people you consider family and to experience belonging and acceptance.
Generosity
To unconditionally share your resources, talents and skills as a way of serving others.
Community Support
To have, or to create, co-operative groups of peers with shared values that provide mutual support and enhancement of each other.
Interdependence
To value personal and inter-institutional co-operation above individual decision-making
Education/ Knowledge
Engaging in ongoing learning to gain new facts, truths, principles and insights.
Service/ Vocation
To use your unique gifts, skills and abilities to contribute to society through your career, profession or calling.
Work
To have the skills, confidence and desire to engage in productive work.
Cooperation/ Reciprocity
To work with others in ways that enable everyone’s unique skills and qualities to supplement, support and enhance each other.
Eight of the top 10 values were common to “End of Life Care” and “Palliative Medicine”, and many of these are relational:
Care / Nurture
Empathy
Family / Belonging
Generosity
Interdependence
Community Support
Education / Knowledge
Service / Vocation
When we shared our initial findings with a group focusing on Co-production in the NHS, people asked an important question: were these values specific to stories relating to end of life care, palliative care and palliative medicine, or were these values generic across other experiences of health care? We did not know the answer so we tried to find out.
For comparison…
We analysed Care Opinion stories about vaccination in the COVID pandemic, seeing this as a very different context to care at the end of life. We found 37 stories about COVID vaccination (2784 words) again the values analysis had something interesting to say. Vaccination stories shared 5 of 10 top values with our results for palliative care/medicine:
Interdependence
Generosity
Empathy
Education / Knowledge
Care / Nurture
Values expressed in stories about COVID vaccination:
Hierarchy/ Protocol
To have a hierarchical arrangement of persons and things in conformity with established levels of authority within an organisation.
Ownership/ Authority
To have ownership of material assets that gives one authority.
Communication/ Information
The effective and efficient flow of ideas and factual information.
Interdependence
To value personal and inter-institutional co-operation above individual decision-making
Generosity
To unconditionally share your resources, talents and skills as a way of serving others.
Health/ Well-being
To practise self-awareness and healthy living in order to have physical and emotional well-being.
Empathy
To deeply relate with others in such a way that they feel understood.
Education/ Knowledge
Engaging in ongoing learning to gain new facts, truths, principles and insights.
Achievement
To accomplish something noteworthy and admirable in your work, education, or your life in general.
Care/ Nurture
To be physically and emotionally supported by family and friends and to value doing the same for others.
We noticed...
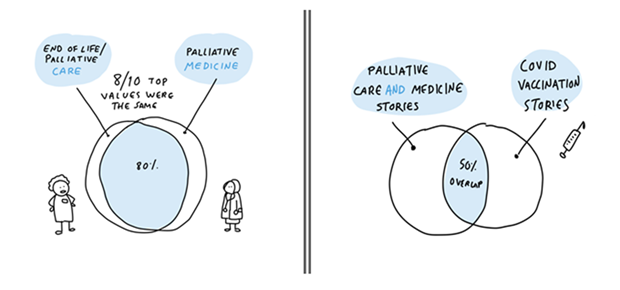
The vaccination stories Top 10 expressed more Control values and they came at the top of the list. Control values are concerned with how well things are organised and how efficiently things are done. Even though Control values came through more strongly, it remained clear that the nature or tone of the interaction still mattered, and what mattered about the interaction is the same as in end of life care, palliative care, palliative medicine.
Interdependence is common to all:
to value personal and inter-institutional co-operation above individual decision-making.
All of this left us with another question.
What can we do to try and create conditions for these values to thrive? Might we be able to deliberately harness these values, to set the tone and create connection between those who provide care and those for whom effective care is key?
We explore this is in our next blog and hope you will join us here.
Thanks for reading!
What do you think? We’d love to hear from you. Drop us a line in the comments below or join in the conversation on Twitter. You can reach us at
Thanks to NHS Dorset for funding this work, colleagues at Dorset Healthcare University Foundation Trust, University Hospitals Dorset NHS Foundation Trust, Lewis-Manning Hospicecare, Forest Holme Hospice Charity, Care Opinion, Magma Effect, Tracy Hixson and all who have shared their experiences.
Illustrations by Virpi Oinonen.
Values inside stories
Values inside stories https://careopinionuk-staging.azurewebsites.net/resources/blog-resources/107-images/296900e5927f4a1aa7e2531d428f3898.png Care Opinion 0114 281 6256 https://www.careopinion.org.uk /content/uk/logos/co-header-logo-2020-default.pngUpdate from Poole Hospital Palliative Care Service
Posted by Saskie Dorman, Consultant in Palliative Medicine, Forest Holme Hospice, University Hospitals Dorset NHS Foundation Trust, on
Thanks for your feedback.